What is ectropion?
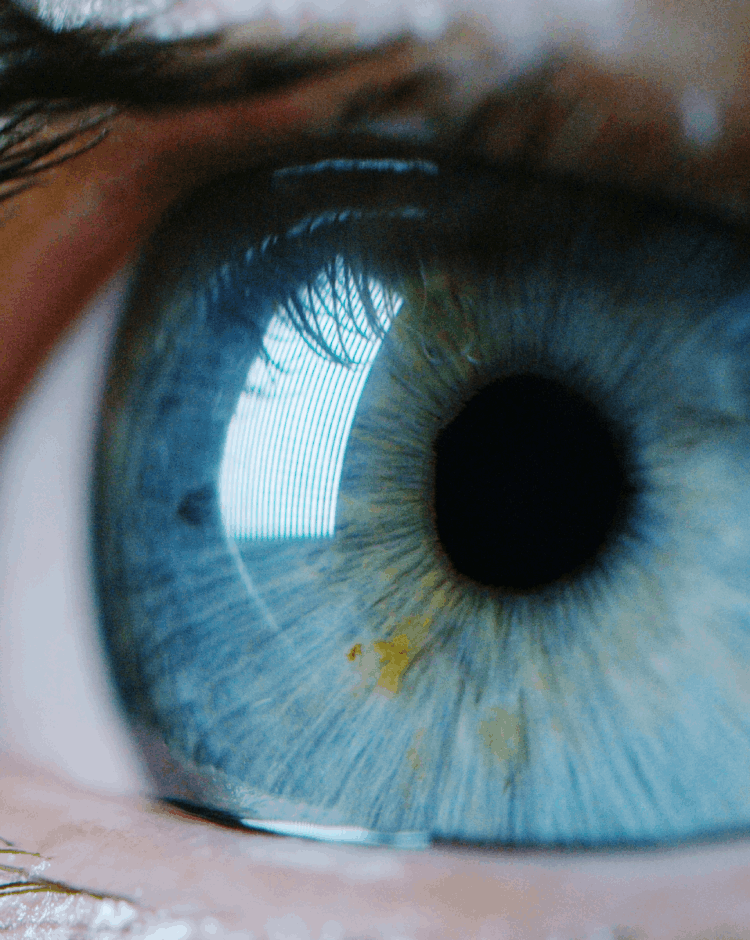
Ectropion is a condition in which the lower eyelid turns outward, exposing the inner part of the eyelid. This outward eversion can lead to irritation, excessive tearing, and a feeling of dryness. In severe cases, ectropion may cause repeated eye infections, corneal damage, or even ulceration, impacting overall eye health.
Ectropion commonly affects the lower eyelid, particularly in older adults, due to age-related laxity in the eyelid muscles and surrounding tissues. However, it can also be congenital (present at birth), though this is much less frequent.
Ectropion symptoms may vary from mild irritation and watery eyes to more pronounced signs such as constant tearing, redness, and sensitivity to light. Artificial tears and lubricating ointments may help temporarily alleviate symptoms, but ectropion surgery is recommended for long-term relief and eyelid malposition correction.
What are the types and causes of ectropion?
Ectropion can be divided into several types, each with distinct causes. Some forms are age-related, as the eyelid’s structural support weakens over time, while others result from factors like trauma, nerve damage, or inflammatory conditions.
Involutional ectropion: caused by age-related weakening of the eyelid’s structural support, leading to the outward turning of the lower eyelid. Typically developing around age 60 and beyond, this condition occurs as facial muscles, tendons, and ligaments lose strength and elasticity.
Cicatricial ectropion: caused by skin scarring, which pulls the eyelid outwards. Burns, trauma, previous eyelid surgery and skin conditions, including rosacea, can all have this effect.
Paralytic ectropion: caused by facial paralysis damage to the innervation of the muscles that supply the eyelid, usually seen following Bell’s palsy, facial nerve palsy.
Mechanical ectropion: caused by the weight of a mass pulling the lower eyelid down and outwards.
Congenital ectropion: caused when the lower lid margin has been turned outwards since birth and is the rarest type of ectropion.
Ectropion after blepharoplasty: this is a very complex problem to treat and can be due to all the above causes. Please see the revision blepharoplasty page for more details on how this can be approached.
Understanding the specific type of ectropion is essential for determining the appropriate ectropion treatment and ensuring effective relief from symptoms.