FAQ
What are the risks and side effects of orbital decompression surgery?
As with almost any surgery, there’s a risk of infection or bleeding, though this is rare. You can also experience eyelid swelling and possible light scarring.
How much does the surgery cost?
The cost of your surgery will vary significantly depending on the type of treatment required. Following your consultation, we will provide a detailed breakdown of the costs tailored to your specific needs.
Will I have scars after the treatment?
The likelihood of scarring depends on the surgical approach. Endoscopic procedures for decompression usually leave no visible scars. However, other types of surgery may result in scars, which are generally small and discreetly placed to minimise visibility.
How can I relieve the burning in my eyes?
Artificial tears or eye drops are good for this. Your specialist will be able to advise you.
How can I reduce the appearance of swelling?
Sleeping with your head elevated is a good approach to prevent fluid buildup, and try to reduce your salt intake.
Does nutrition have an effect on thyroid eye disease?
It certainly can. A healthy and balanced diet without excess salt is best for those with TED. Selenium supplementation is also beneficial for mild TED.
Can smoking increase the risk of having TED?
100%. Smoking can double or even triple your chances of acquiring TED much more than that of a non-smoker.
Will I require further surgery?
It’s impossible to say until the initial treatments are carried out and the results observed. Some patients may require follow-up surgeries.
Does orbital decompression surgery correct double vision?
It can, but double vision may also persist even with surgical intervention. Additional eye muscle surgeries or other approaches, like patching, can help with this.
Is it contagious?
Not at all.
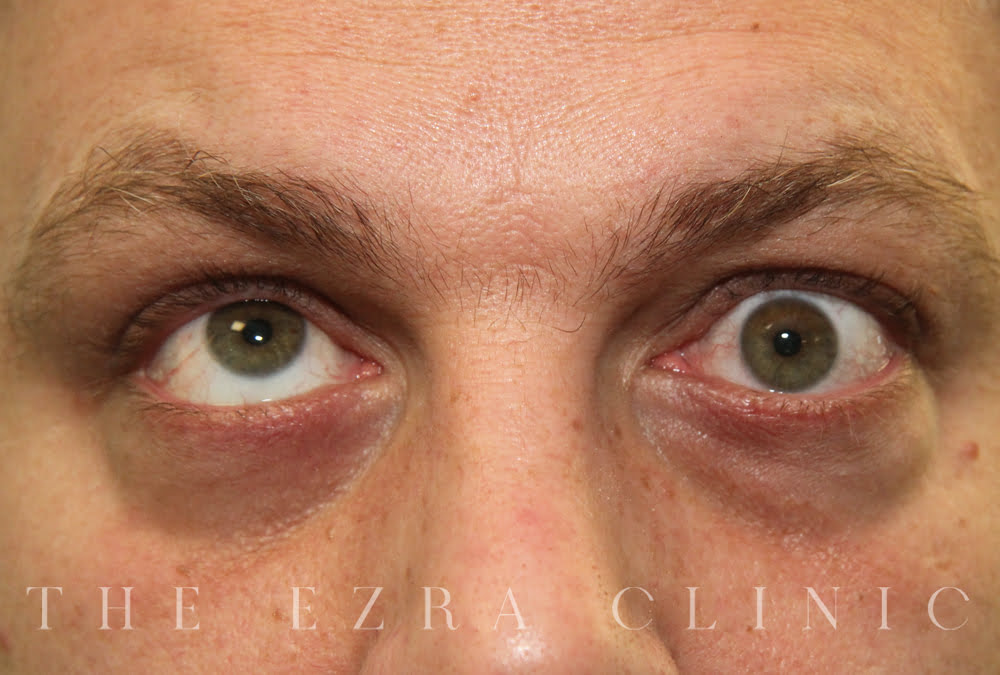
What causes my eyes to bulge when I have TED?
It’s related to the swelling of sections of muscle and tissue behind and around the eyeball that essentially pushes the eye forward.